Who Has Had Eustachian Tube Balloon Dilation Reviews
- Original research article
- Open Access
- Published:
Airship dilation of the eustachian tube: a tympanometric outcomes assay
Journal of Otolaryngology - Caput & Cervix Surgery volume 45, Article number:13 (2016) Cite this article
Abstract
Groundwork
Eustachian tube dysfunction (ETD) is a common medical issue, occurring in at least i % of the adult population. Patients suffering from ET dysfunction typically present with complaints of hearing loss or sensation of pressure or plugged ear, which tin pb to impaired quality of life. Over time ETD tin consequence in conductive hearing loss or choleastatoma formation. Effective theraputic options for ET dysfunction are few. Eustachian tube balloon dilation is a novel surgical technique existence used to treat ETD.
The aim of our report is to objectively measure the success of Eustachian tube airship dilation by comparing pre and mail-operative middle ear pressures using tympanometric testing.
Methods
RA retrospective nautical chart review was preformed on all patients who underwent balloon dilation of the Eustachian tube by authors NC or MB from 2010 to 2014. Pre and mail-operative tympanograms were analyzed and categorized based on type (Type A, Type B, Type C). Success was defined past an comeback in tympanogram blazon: Blazon B or C to Type A, or Type B to blazon C. Pre and mail service-operative tympanograms were farther analyzed using eye ear pressure values. Follow-up ranged from 3 to fifteen months.
Results
20-5 ears (eighteen patients) were included in the study. Overall 36 % of ears had improvement in tympanogram type, and 32 % had normalization of tympanogram post-operatively. The Jerger tympanogram type improved significantly following the procedure (p = 0.04). Patients also had statistically significant improvement in measured centre ear pressure mail service-operatively (P = 0.003).
Conclusion
The natural history of Eustachian tube dysfunction is poorly understood, and prove for current treatments are limited. Eustachian tube balloon dilation is a safe procedure, and produces significant improvement in tympanogram values upwardly to 15 months post-operatively. Farther refinement of patient option and standardization of technique is required to optimize the event of this therapy. Longterm follow-up data will clarify the persistence of the event.
Background
The Eustachian tube (ET) is a conduit betwixt the middle ear space and the nasopharynx, which opens in a physiologically complex and poorly understood way to provide ventilation to the eye ear, then equalize middle ear and ambient pressures. In this report, we refer by "Eustachian tube dysfunction" only to dilatory Eustachian tube dysfunction, i.e. failure to open and ventilate the heart ear, as opposed to patulous Eustachian tube, in which there is failure of closure of the Eustachian tube. Eustachian tube dysfunction is a common medical upshot, occurring in at least 1 % of the developed population [1]. ET dysfunction can lead to dumb quality of life due to persistent awareness of ear fullness, ear pain, and inability to tolerate air travel or scuba diving. With time, ET dysfunction can pb to conductive hearing loss and cholesteatoma formation.
Patients suffering from ET dysfunction typically present with complaints of hearing loss or sensation of pressure or plugged ear, which tin can be chronic or recurrent. Findings of ET dysfunction can include serous effusion, conductive hearing loss (on tuning fork or audiometric testing), or negative center ear pressure (on pneumatic otoscopy or tympanometry). Later, there may be findings of sequelae of this dysfunction, such equally retraction pockets, perforations, chronic drainage or cholesteatoma. The underlying etiology and natural history of ET dysfunction is poorly understood. There is a lack of clear diagnostic criteria, which further impairs our power to study the affliction and potential therapies. Anti-reflux therapy or nasal steroid sprays are often used start line treatments, without much evidence to support their efficacy. A randomized, placebo controlled study examining the result of nasal steroid spray on ET dysfunction establish no significant difference between treatment and placebo [2]. Similarly, a recent systematic review found no pregnant consequence of any intervention including observation, nasal steroids, and various surgical techniques [iii].
The standard surgical treatment of ET dysfunction is myringotomy and tympanostomy tube placement in the tympanic membrane (TM). This technique allows equalization of middle ear force per unit area and drainage of fluid via the TM, finer bypassing the ET. This approach effectively relieves symptoms but does not treat the ET dysfunction. Tympanostomy tubes often need to be replaced multiple times if ET dysfunction persists. This places a burden on the health care system and adds to patient discomfort and inconvenience. Tympanostomy tubes also take some risk of perforations of the tympanic membrane, with associated conductive hearing loss. Other novel surgical therapies accept emerged, which focus on the ET itself.
In select patients there is redundant mucosa in the area of the opening of the ET, impairing its dilation. Ablation of this tissue with laser [iv] or microdebrider [v] has shown promise in pocket-size studies merely these interventions are not advisable for all patients. Other novel therapies have focused on the cartilaginous portion of the ET [6]. Of detail note, a recent, promising innovation is airship dilation of this portion of the ET.
Eustachian tuboplasty by balloon dilation involves the cannulation of the cartilaginous portion of the ET via the nasopharynx with a balloon catheter. This catheter is inflated to multiple atmospheres of pressure (typically ten–12 bar) for a brusque amount of time and then removed. The surgical technique is also variable in the literature. Balloons used range between 3–7 mm in bore, and are of variable lengths. They are typically inflated for 1–2 min. Currently, no show exists regarding the optimal airship bore, pressure, or elapsing of inflation.
Numerous studies have demonstrated the safety of this procedure. A systematic review preformed in 2014 showed no adverse outcomes in 103 patients who had undergone airship dilation of the Eustachian tube [iii]. While some brusque term success has been reported, there is trivial data regarding long-term outcomes [7–12]. The criteria for measuring surgical success are inconsistent across studies, with outcomes oftentimes consisting of subjective symptomatic impressions or non-validated subjective scoring systems. The main outcome for the present report was middle ear pressure level comeback following ET dilation in patients with chronic ET dysfunction. This was accomplished past comparison pre- and post-operative tympanogram values.
Methods
Approval for this study was obtained from our Nova Scotia Health Potency Research Ethics Lath. Information were collected via retrospective chart review. All patients who underwent balloon ET dilation past authors NC or MB, from 2010 to 2014, were reviewed. The procedures were preformed at 2 different centers but the surgical technique was consequent. The Belfiel® Eustachian tube dilatation system (Spiggle and Theis, Overath, Federal republic of germany) was used. Nether full general anesthesia the Eustachian tube orifice was identified endoscopically, and cannulated with a 20 mm long, three mm bore balloon. The airship was inflated for two min at 10 bar and then removed. Surgeon MB also placed tympanostomy tubes in a subset of patients. These patients were not selected, just rather requested concurrent placement of tympanostomy tubes, as this was the standard therapy they were accustomed to. In that location was no other option benchmark for patients who received a ventilation tube and those who did not.
Patients were selected for ET balloon dilation if they had long-standing Eustachian tube dysfunction (ETD) treated with multiple sets of tympanostomy tubes, and were interested in pursuing a longer-term solution. Patients were excluded from analyses if they had a normal pre-operative tympanogram or an 'open' post-operative tympanogram (i.e., a perforation or patent tympanostomy tube). These patients could not exist included as a primary event measure out was improvement on the tympanogram, which couldn't be measured for comeback in these cases. If the tympanostomy tube extruded or the perforation healed during the report period, the results were included in analysis. Patients were also excluded if no post-operative tympanograms were performed.
Tympanogram results were collected retrospectively from pre-operative visits and all visits upwards to fifteen months post-operatively. Follow up time points were 2–3 months, 6–nine months, and 12–15 months post operatively. In-hospital audiologists preformed Tympanometric testing. Values were generated using a tympanometer, which produced waveforms and top pressure values. Tympanograms were then assessed past audiologists (blinded) and again past the attending surgeon (not blinded). Although standard definitions of Type A, B and C tympanograms were used, there is the possibility of estimation bias. The pre-operative and well-nigh recent post-operative tympanograms were categorized based on blazon (Type A, Type B, Type C) and compared using the Wilcoxon Signed Rank Test. Success was divers by an improvement in tympanogram type: Type B or C to Blazon A, or Type B to type C.
Data analysis
Each patient was analyzed by comparing their pre-operative tympanogram and their most contempo post-operative tympanogram value. The data was broken down for two different analyses. First, the change in tympanogram Jerger type was analyzed, as this is the most clinically familiar parameter. For this, we counted how many tympanograms evolved from ane blazon (A, B, or C) to some other type post-treatment. Information for a 2d assay were regrouped to better assess the Blazon C tympanograms, by analyzing by the actual measured eye ear force per unit area before and after balloon dilatation. Blazon C tympanograms were defined every bit those with the maximum compliance tiptop at less than -150 dPa. The negative tympanogram values were grouped past 100 daPa intervals. This was assessed commencement for all patients, (i.e those who did, and did not, receive ventilation tubes in amass). Then we repeated the analysis for just the subset that had received ventilation tubes meantime. This was performed, despite the low numbers, so that nosotros could see if this group had dissimilar outcomes compared to the group without concurrent ventilation tubes. Tympanograms for this subset were preformed after the tubes had extruded and the tympanic membrane had healed, not while the tubes were in place. The data were not-parametric, repeated measures and then a Wilcoxon Signed rank test was selected to make up one's mind statistical significance. Type B tympanograms do not generate a numerical value so our data set could not be analyzed using parametric tests.
Results
A full of 25 ears were included. Patients ranged in historic period from 18–68 years, with a hateful age of 40.half dozen years. Follow-upward time ranged from 3 to xv months with a hateful follow-up of vii.1 months. All patients had recurrent serous otitis media or negative pressure and retraction, requiring ventilation tube insertions. Nine patients underwent bilateral operations (xviii ears), and half dozen patients had had previous tympanostomy tube insertion. Previous mastoid surgery or tympanoplasty had been preformed on 4 patients.
Tympanograms were preformed at each follow upwards visit, and the nearly recent post-operative tympanograms were used for assay. A summary of the results experienced by individual patients is summarized in Table ane. Overall, 36 % of patients improved their tympanogram type and 32 % had their tympanogram normalize to Type A. Effigy ane shows pre-operative and post-operative results past tympanogram type. The type improved significantly following the procedure (p = 0.04). Figure 2 illustrates the results with negative tympanograms (type C) categorized by 100 daPa intervals. Effigy 2 appears to prove a clearer difference betwixt pre and post operative condition. Again, the improvement was significant (p = 0.003). At one eye, 5 of 11 ears had concurrent tympanostomy tube placement with ET dilation. In this group, 60 % had normalization of middle ear pressure. In the remaining half-dozen of eleven ears, 67 % improved in tympanogram type and fifty % normalized. Data on the timing of tympanostomy tube extrusion was not available. Figure iii illustrates the proportion of abnormal tympanograms pre operatively and at multiple post operative follow upwards points. The proportion of aberrant tympanograms was highest pre-operatively and decreased almost between pre operative and 2–3 month follow up points. All follow upwards points had a lower proportion of abnormal tympanograms compared to preoperative measures. This was generated through tympanometric analysis at all follow upwards points. The almost negative centre ear pressure pre operatively (due north = 18, mean = −295 DaPa, SD = 77.38) with the most improvement seen at the 2-3 calendar month follow up point (n = 15, hateful = −164 DaPa, SD = 105.09). Heart ear pressure at 6–ix months (n = nine, mean = −255, SD = ninety.08) and at 12-15 months (northward = 8, mean = −213, SD 124.64) besides remained less negative compared to pre-operative state.
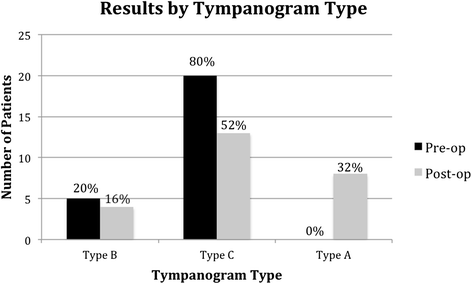
Pre and post-operative assessment of tympanogram type
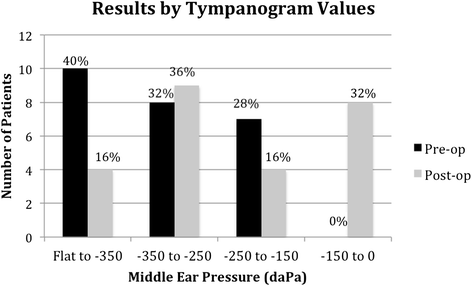
Pre and post-operative grouped tympanogram values
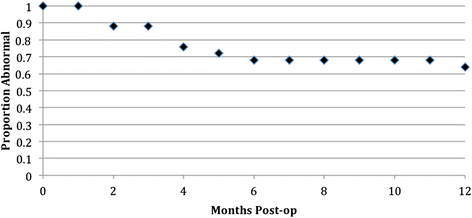
Kaplan Meier survival curve of proportion of abnormal tympanograms at various follow-upward points
No adverse events occurred as a result of ET balloon dilation.
Give-and-take
Eustachian tube balloon dilation has emerged as a surgical option, which targets the cartilaginous portion of the ET. Histopathological analysis preformed after balloon dilation shows decreased inflammation in the surface epithelium and submucosal tissues. The net reduction of inflammation is the hypothesized mechanism for improvement in clinical Eustachian tube part post-operatively [5]. Recent studies accept shown promise in both brusque term and long-term outcomes, but variability in operative arroyo, sample size, patient follow-up, and outcome measurements make it difficult to interpret with certainty [3, 6–12]. Many studies focus not on tympanometric outcomes, simply on power to valsalva, opening pressures, or subjective outcomes. We experience the most important stop-bespeak is whether or not there is return of heart ear ventilation, and have used middle ear pressure as a surrogate measure out for this. Our study relied on objective measurements using tympanogram values, and had follow-up to xv months post operatively.
Overall, 36 % of patients showed an improvement in tympanogram type post-operatively (Table 1) and this improvement was pregnant (p = 0.04, Fig. 1). Similarly, tympanogram measurement categorized by 100 daPa intervals likewise showed statistically meaning improvement post-operatively (p = 0.003, Fig. 2). Follow-up time ranged from three to xv months with a mean follow-upwards of vii.i months, and the most recent mail-operative tympanograms were used for analysis. A recent systematic review of Eustachian tube airship dilation showed a conversion to type A tympanograms in 36 to 96 % of patients [3]. Silvola et. al reported type A tympanograms in 23 (56 %) patients post operatively, compared to ane (2 %) pre-operatively, with a similar follow-up time [7]. The bottom benefit in found our study might exist due to variability in patient selection, or surgical arroyo. Silvola et. al reported use of a 7 mm diameter balloon, whereas nosotros used a 3 mm balloon.
Other studies of involvement reported outcomes in a summative Eustachian Tube Score (ETS). This score relies on subjective symptoms and tubomanometry to measure successful opening of the Eustachian tube mail service-operatively with pressurization of the nasopharynx. A higher score indicates comeback in subjective symptoms and lower opening pressures on tubomanometry. For 1076 balloon dilation procedures, Schroder et. al found significant improvement in 71 % of patients at two months mail service-operatively, 73 % at 1 twelvemonth, and 82 % at 2 years procedures [viii]. In a study of 380 cases, Dalchow et. al also showed a hateful increase in ETS at 12 months post-operatively [nine].
We nowadays the first Canadian data on balloon dilatation of the ET. In our written report, the concurrent placement of tympanostomy tubes at the time of ET dilation does not appear to meliorate outcomes, though sample size of those who received a ventilation tube was small. No literature has shown outcomes of ET balloon dilation with concurrent myringotomy.
Limitations of our report include relatively small sample size, limited longitudinal follow upwardly, and lack of a control group. Due to these limitations, and the lack of a control arm in our study, we cannot say, definitively, if our intervention improved ET part over fourth dimension, compared to simple ascertainment.
The use of objective outcome measurements is strength of the study, nevertheless, nosotros did non collect associated subjective outcomes. Thus, while some middle ear pressures improved, nosotros cannot say if this was related to relief of symptoms or improved quality of life. This consideration would be important for future studies.
Other future directions of this written report include the effect of adjunctive interventions (i.due east., tympanostomy tube insertion) preformed at the time of Eustachian tube airship dilation and determining if at that place are patient factors that correlate with success. Further analysis of surgical protocol and equipment will aid in comparing of results amid studies and improve the predictability of patient outcomes. It is of import for clinicians to document their results with unlike diameter balloons, airship pressures, and dilatation times, so that these parameters tin be compared and the surgical approach optimized for success.
Decision
Eustachian tube dysfunction is a common entity that is hard to treat. Eustachian tube balloon dilation produces modest comeback in tympanogram scores up to 14 months postal service-operatively. Further refinement of patient choice and standardization of technique is required to optimize the effect of this therapy.
Abbreviations
- CSOM:
-
Chronic serous otitis media
- ET:
-
Eustachian tube
- ETD:
-
Eustachian tube dysfunction
- TM:
-
Tympanic membrane
References
-
Browning GG, Gatehouse S. The prevalence of middle ear illness in the adult British population. Clin Otolaryngol Allied Sci. 1992;17:317–21.
-
Gluth MB, McDonald DR, Weaver AL, Bauch CD, Beatty CW, Orvidas LJ. Management of eustachian tube dysfunction with nasal steroid spray: a prospective, randomized, placebo-controlled trial. Curvation Otolaryngol Head Neck Surg. 2011;137:449–55.
-
Llewellyn A, Norman G, Harden M, et al. Interventions for adult Eustachian tube dysfunction: a systematic review. Wellness Technol Assess. 2014;18(46):one–180.
-
Caffier PP, Sedlmaier B, Haupt H, Göktas O, Scherer H, Mazurek B. Touch on of laser eustachian tuboplasty on middle ear ventilation, hearing, and tinnitus in chronic tube dysfunction. Ear Hear. 2011;32:132–9.
-
Metson R, Pletcher SD, Poe DS. Microdebrider eustachian tuboplasty: A preliminary written report. Otolaryngol--Caput Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2007;136:422–7.
-
Kivekäs I, Chao WC, Faquin Westward, et al. Histopathology of airship-dilation Eustachian tuboplasty. Laryngoscope. 2015;125(2):436–41.
-
Silvola J, Kivekäs I, Poe DS. Airship Dilation of the Cartilaginous Portion of the Eustachian Tube. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Cervix Surg. 2014;151:125–xxx.
-
Schröder Southward, Lehmann M, Ebmeyer J, Upile T, Sudhoff H. Airship Eustachian Tuboplasty (BET): our experience of 622 cases. Clin Otolaryngol. 2015. doi:ten.1111/coa.12429. [Epub alee of print] PubMed PMID: 25867023.
-
Dalchow CV, Loewenthal M, Kappo N, Jenckel F, Loerincz BB, Knecht R. First results of Endonasal dilatation of the Eustachian tube (EET) in patients with chronic obstructive tube dysfunction. Eur Arch Otorhinolaryngol. 2015. [Epub ahead of print] PubMed.
-
Catalano PJ, Jonnalagadda S, Yu VM. Airship catheter dilatation of Eustachian tube: a preliminary report. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. 2012;33:1549–52.
-
Jurkiewicz D, Bień D, Szczygielski K, Kantor I. Clinical evaluation of balloon dilation Eustachian tuboplasty in the Eustachian tube dysfunction. Eur Arch Oto-Rhinoceros-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. 2013;270:1157–60.
-
Ockermann T, Reineke U, Upile T, Ebmeyer J, Sudhoff HH. Balloon dilatation Eustachian tuboplasty: a clinical study. Laryngoscope. 2010;120:1411–vi.
Author information
Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BW preformed retrospective review, analysis, refined and edited manuscript. BT preformed writing of manuscript and formatting. NC provided guidance for the written report. MB provided guidance for the study, assisted with manuscript. All authors read and approved the final manuscript.
Authors' information
BW is a Senior Resident in the Partition of Otolaryngology – Head and Neck Surgery at Dalhousie University, Halifax, Nova Scotia. BT is a Inferior Resident in the Division of Otolaryngology – Caput and Neck Surgery at Dalhousie University, Halifax, Nova Scotia. NC is an Otolaryngologist, Banana Professor, and Head of Surgery at St Martha'due south Regional Infirmary, Antigonish, Nova Scotia. MB is an Otologist/Neurotologist, Professor and Division Head of Otolaryngology – Caput and Cervix Surgery at Dalhousie University, Halifax, Nova Scotia.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/past/4.0/), which permits unrestricted utilise, distribution, and reproduction in any medium, provided you give advisable credit to the original author(southward) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/ane.0/) applies to the information made available in this article, unless otherwise stated.
Reprints and Permissions
Virtually this article
Cite this article
Williams, B., Taylor, B.A., Clifton, North. et al. Balloon dilation of the eustachian tube: a tympanometric outcomes assay. J of Otolaryngol - Head & Neck Surg 45, xiii (2016). https://doi.org/x.1186/s40463-016-0126-6
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s40463-016-0126-vi
Keywords
- Eustachian tube
- Eustachian tube balloon dilation
- Balloon dilation
- Eustachian tube dysfunction
- Tuboplasty
Source: https://journalotohns.biomedcentral.com/articles/10.1186/s40463-016-0126-6
Post a Comment for "Who Has Had Eustachian Tube Balloon Dilation Reviews"